#Cellulitis skin infection
Explore tagged Tumblr posts
Text
cellulitis treatment: quick relief | KBK Hospitals

Quick and effective cellulitis treatment at KBK Hospitals. Precise diagnosis, holistic care, and customized plans for fast recovery
#Cellulitis skin infection#Antibiotics for cellulitis#Cellulitis symptoms#cellulitis prevention#cellulitis diagnosis#cellulitis cure#skin infection treatment
0 notes
Text
sometimes you have a rough week with several migraines, and its like. man that mild traumatic brain injury sure does keep hitting!
and then it doesn't stop hitting. so you go to urgent care after work and surprise! you have cellulitis.
#2000mg of cephalexin a day cellulitis :)#and Also bursitis!#because two is twice the fun i guess#love the UC visits that take ten minutes bc the doc takes one look and goes WHOA HEY BUDDY LETS STOP THAT#it doesnt happen often but every time a UC doc looks at me and gets real big eyes. i feel validated.#havent actually had that happen since The Lung Infection in early 2019. very exciting!#several of my coworkers today were giving me Looks like Why Are You Still Here and the answer is#because i was raised by a woman who did Not go to the dr for Anything. thank u mum.#i wasnt actively dying so i went to work. when the skin got HOT to the touch is when i started worrying#and when my coworkers started whale eyeing me it was like OKAY OKAY OKAAAAY IM GOIIIIING IM GOING AFTER WORK#working in the medical field has been very Enlightening
3 notes
·
View notes
Text
Acute Bacterial Skin And Skin Structure Infections Market Trends driven by Increasing Antibiotic Resistance
The acute bacterial skin and skin structure infections (ABSSSI) market comprises anti-infective drugs that are used to treat skin infections caused by bacteria. These infections include impetigo, cellulitis, wound infections, and major cutaneous abscesses. The commonly prescribed drugs are antibiotics such as cephalosporins, carbapenems, lipoglycopeptides, oxazolidinones, and tetracyclines. The increasing threat of antimicrobial resistance (AMR) has boosted the demand for effective antibiotic treatments. Growing prevalence of skin infections owing to rising environmental pollution levels and lifestyle changes has also augmented market growth.
Global acute bacterial skin and skin structure infections market is estimated to be valued at USD 3,842.5 Mn in 2024 and is expected to reach USD 5,701.7 Mn by 2031, exhibiting a compound annual growth rate (CAGR) of 5.8% from 2024 to 2031.
Key Takeaways Key players operating in the Acute Bacterial Skin And Skin Structure Infections market are Fresenius SE and Co. KGaA, Pfizer, Inc., Amneal Pharmaceuticals LLC, Intas Pharmaceuticals Ltd., Cadila Healthcare Ltd., Glenmark Pharmaceuticals Ltd, GSK plc, Sun Pharmaceutical Industries Ltd., Aurobindo Pharma Ltd., AbbVie, Inc., Melinta Therapeutics LLC, Accord Healthcare Ltd., Merck and Co., Inc., Teva Pharmaceutical Industries Ltd., Paratek Pharmaceuticals, Inc. The growing prevalence of skin infections across the world coupled with the rising threat of AMR is fueling the demand for effective antibiotic therapies. Leading market players are investing in R&D to develop novel drugs with new mechanisms of action. On the other hand, companies are also undertaking initiatives to expand their presence in emerging economies through strategic partnerships and acquisition activities. The Acute Bacterial Skin And Skin Structure Infections Market Demand rising threat of antimicrobial resistance is a key concern that is augmenting the demand for novel and effective anti-infective treatments for ABSSSIs. According to the WHO, drug-resistant bacteria could cause 10 million deaths annually by 2050 if adequate actions are not taken. Growing awareness regarding antibiotic stewardship practices is reducing the irrational use of antibiotics to some extent. However, further regulatory interventions and strict prescribing guidelines are required to curb the development and spread of resistant pathogens. Market Key Trends One of the major trends witnessed in the acute bacterial skin and skin structure infections market is the rising focus on developing new antibiotic classes with novel mechanisms of action to overcome anti-microbial resistance. Several pipeline drugs under clinical trials employ new mechanisms like inhibition of bacterial DNA/RNA synthesis, cell wall biosynthesis, and protein synthesis. Monoclonal antibodies targeting specific toxins produced by resistant bacteria is another novel area being explored. Fast track approvals and commercialization of path-breaking antibiotic therapies will ensure long-term market sustenance amid growing healthcare costs and stringent pricing control by governments globally.
Porter's Analysis Threat of new entrants: New players find it difficult to enter this market owing to high costs of R&D and regulatory requirements. Bargaining power of buyers: Many buyers have low bargaining power due to lack of alternatives. Bargaining power of suppliers: Suppliers have moderate bargaining power due to availability of substitute sources. Threat of new substitutes: Threat from new substitutes is moderate due to technology developments and increasing investments in alternatives. Competitive rivalry: Fierce competition exists among existing players to gain market share. Geographical Regions North America accounts for the largest share of the global acute bacterial skin and skin structure infections market, in terms of value, followed by Europe. This is attributed to the rapidly growing incidence of skin infections, advanced healthcare infrastructure, favorable reimbursement policies, and high awareness among healthcare professionals and patients regarding diagnosis and treatment. Asia Pacific is expected to witness the fastest growth during the forecast period, primarily driven by improving access to healthcare facilities owing to rising disposable incomes, growing incidence of skin infections due to changing lifestyles, and supportive government policies and initiatives in emerging economies. Rising medical tourism in Asian countries has also boosted the market growth in the region.
Get more insights on Acute Bacterial Skin And Skin Structure Infections Market
Vaagisha brings over three years of expertise as a content editor in the market research domain. Originally a creative writer, she discovered her passion for editing, combining her flair for writing with a meticulous eye for detail. Her ability to craft and refine compelling content makes her an invaluable asset in delivering polished and engaging write-ups.
(LinkedIn: https://www.linkedin.com/in/vaagisha-singh-8080b91)

#Coherent Market Insights#Acute Bacterial Skin And Skin Structure Infections Market#Acute Bacterial Skin And Skin Structure Infections#Cellulitis#Abscess#Skin Abscess#Wound Infection#Erysipelas
1 note
·
View note
Text
Cellulitis
Cellulitis may spread rapidly. Affected skin appears swollen and red and may be hot and tender.
0 notes
Text
Writing Notes: Bites & Stings

References (Dog Bites; Cat; Human; Spider; Bee & Wasp; Snake; Jellyfish)
Bites and stings - puncture injuries inflicted by an animal that penetrate the skin.
DOGS
A typical dog bite results in a laceration, tear, puncture, or crush injury.
Bites from large, powerful dogs may cause fractures and dangerous internal injuries. Dogs trained to attack may bite repeatedly during a single episode.
Infected bites usually cause pain, cellulitis (inflammation of the connective tissues), and a pus-filled discharge at the wound site within 8–24 hours.
Many infections are confined to the wound site, but some of the microorganisms in the mouths of dogs can cause systemic and possibly life-threatening infections.
Rabies is rare among pet dogs in the United States, most of which have been vaccinated against the disease. Tetanus is also rare but can be transmitted by a dog bite if the victim is not immunized.
CATS
The mouths of cats and dogs contain many of the same microorganisms.
Cat scratches and bites are also capable of transmitting the Bartonella henselae bacterium, which can lead to cat-scratch disease, an unpleasant but usually not life-threatening illness.
Cat bites are mostly found on the arms and hands.
Sharp cat teeth typically leave behind a deep puncture wound that can reach muscles, tendons, and bones, which are vulnerable to infection because of their comparatively poor blood supply.
This is why cat bites are much more likely to become infected than dog bites.
Also, people are less inclined to view cat bites as dangerous and requiring immediate attention; the risk that infection has set in by the time a medical professional is consulted is thus greater.
HUMANS
Humans bites result from fights, sexual activity, medical and dental treatment, and seizures. Bites raise the possibility of spousal or child abuse.
Children often bite other children, but those bites are hardly ever severe.
Human bites are capable of transmitting a wide range of dangerous diseases, including hepatitis B, syphilis, and tuberculosis.
Human bites fall into two categories:
Occlusional (true) bites present a lower risk of infection.
Clenched-fist injuries, which are very infectious and can permanently damage the hand, usually result from a fist hitting teeth during a fight.
People often wait before seeking treatment for a clenched-fist injury, with the result that about half of such injuries are infected by the time they are seen by a medical professional.
SPIDERS
As a rule, people rarely see a black widow bite, nor do they feel the bite as it occurs. The first (and possibly only) evidence that a person has been bitten may be a mild swelling of the injured area and two red puncture marks.
Within a short time, some victims begin to experience severe muscle cramps and rigidity of the abdominal muscles. Other possible symptoms include excessive sweating, nausea, vomiting, headaches, and vertigo, as well as breathing, vision, and speech problems.
A brown spider’s bite can lead to necrotic arachnidism, in which the tissue in an area of up to several inches around the bite becomes necrotic (dies), producing an open sore that can take months or years to disappear.
In most cases, the bite simply produces a hard, painful, itchy, and discolored area that heals without treatment in 2–3 days.
The bite may be accompanied by a fever, chills, edema (an accumulation of excess tissue fluid), nausea and vomiting, dizziness, muscle and joint pain, and a rash.
BEES & WASPS
The familiar symptoms of bee and wasp stings include pain, redness, swelling, and itchiness in the area of the sting.
Multiple stings can have much more severe consequences, such as anaphylaxis, a life-threatening allergic reaction that occurs in hypersensitive persons.
SNAKES
Venomous pit viper bites usually begin to swell within 10 minutes and sometimes are painful.
Other symptoms include skin blisters and discoloration, weakness, sweating, nausea, faintness, dizziness, bruising, and tender lymph nodes.
Severe poisoning can lead to tingling in the scalp, fingers, and toes; muscle contractions; an elevated heart rate; rapid breathing; large drops in body temperature and blood pressure; vomiting of blood; and coma.
Many pit viper and coral snake bites (20–60%) fail to poison (envenomate) their victim, or introduce only a small amount of venom into the victim’s body.
The wounds, however, can still become infected by the harmful microorganisms that snakes carry in their mouths.
Coral snake bites are painful but may be hard to see.
One to seven hours after the bite, a bitten person begins to experience the effects of the venom, which include tingling at the wound site, weakness, nausea, vomiting, excessive salivation, and irrational behavior.
Major nerves of the body can become paralyzed for 6–14 days, causing double vision, difficulty swallowing and speaking, respiratory failure, and other problems.
Six to eight weeks may be needed before normal muscular strength is regained.
JELLYFISH
Jellyfish venom is delivered by barbs called nematocysts, which are located on the creature’s tentacles and penetrate the skin of people who brush up against them. Instantly, painful and itchy red lesions usually result.
The pain can continue up to 48 hours.
Severe cases may lead to skin necrosis, muscle spasms and cramps, vomiting, nausea, diarrhea, headaches, excessive sweating, and other symptoms.
In rare instances, cardiorespiratory failure may occur.
Source ⚜ More: Writing Notes & References More: Writing Realistic Injuries ⚜ On Anatomy ⚜ Poison ⚜ Fight Scenes Part 1 2
#writing notes#animals#writeblr#dark academia#spilled ink#literature#writers on tumblr#writing reference#writing prompt#medicine#poets on tumblr#poetry#words#writing inspiration#creative writing#fiction#dogs#writing ideas#thomas gainsborough#writing resources
195 notes
·
View notes
Text
Saw a patient today who had been through a series of medical visits that epitomizes what I hate about multiple different kinds of care providers. Their VA dermatologist took a scoop out of them to remove a basal cell cancer. Fine. I’m not a dermatologist, maybe it needed those wide margins. (If it didn’t, going that deep should mean it was an excisional biopsy and they put in sutures to close it.) They gave the patient and his wife confusing instructions about wound care. They didn’t provide guidance around keeping it covered or moist. It got infected. His wife took him to Urgent Care. The UC doc took a swab of the wound and started antibiotics. They came to see me for a visit we scheduled ages ago for something else.
Here’s the thing. Wounds need to be kept at what I call the Goldilocks moisture level: not too dry and not too wet. If it’s pruny/white/mushy like it’s been in a bathtub, it’s too wet. If it’s cracking, it’s too dry. This is why you can’t say “cover it for X days and then leave it out.” That would be like telling someone with heart failure and lower extremity edema “take the diuretic for a week and then stop” without any instructions around dry weight, dizziness, etc. It’s more complicated than that.
This wound was too dry. No one had talked to them about keeping it moist. No one had even mentioned Vaseline.
No, they got a wound swab. Want to guess how good a wound swab is for an open wound exposed to the world? Pretty terrible. You can improve it a little bit by making sure you’ve removed some kind of layer and then expressing fluid directly from the wound with the swab, but it’s still bad. The only time I give a shit about what grows from a wound swab is when it was a) collected in the OR (as when the podiatrist gets a sample of osteomyelitic bone in a sterile environment) or b) when it grows pseudomonas. Everything else? I can figure out by looking at it. If it’s skin it’s probably either staph or strep. If it’s staph, it’s either MRSA or MSSA. If it’s MRSA, it’s making a lot of pus, it’s red, it’s hot, it’s painful. This wasn’t. So it was either MSSA or strep. So what are we going to do for systemic antibiotics? Probably the same thing we would have done anyway—Keflex.
And what’s the utility of systemic antibiotics in a skin wound? Not a lot, most of the time. This wasn’t cellulitis proper. It wasn’t red or hot or angry enough. A red border around the wound does not a systemic infection make. And if you don’t care properly for the wound itself, there’s no point in antibiotics, because it still can’t heal. Antibiotics can get where blood goes. Blood does not go into the slough that is the bacterial biofilm covering a wound.
So I sat there with gauze and saline and gently debrided the 100% slough off the wound. It’s yucky and it takes time and attention. It doesn’t get compensated. That’s why no one else had done it yet. The derm had blown it off as “it’s healing, it’s fine.” It wasn’t healing. It was developing rolled edges, where the wound edges couldn’t heal across the slough and so they started to curl back under themselves. If taking off the slough (and keeping it gone by MAINTAINING PROPER CONDITIONS) doesn’t let it heal, I’ll need to get him back in and rough up the edges with a Buck’s curette until it can heal.
Multiple professionals who should have known better tried to make my patient just go away, rather than heal him.
I’m pissed. I’m tired. I think I have a cold. I shouldn’t be doing the work the dermatologist or the UC provider should have done. And because of everything they’d told her, his wife was pissed at me for doing what was correct. “We’ve heard a lot of different things!” Yes, and I’m right. You’ll find out when the wound actually starts healing when we care for it properly.
The value of a model is in what it can predict. Wounds are great about making it clear when your model sucks.
295 notes
·
View notes
Text
Opposites of Attractions Ch. 4 (Kid x Reader, enemies to lovers)

18+ MDNI | On Ao3
The other chapters
Thank you to @nocturnalrorobin and @limitlesstildil for beta-ing this work <3 <3 <3
Your POV
You had never once turned in a pirate for their bounty - you weren’t a bounty hunter, you were a mercenary. You admired their dedication to fighting for their dreams, their complete refusal to live within the bounds of society. But if you passed a Marine base in the next ten minutes, you’d be encapsulating the ship and everyone in it in iron and tossing them to the Marines, free of charge.
Since you’d reluctantly accepted Kid’s demand that you be their nurse, you’d seen a steady stream of the crew coming to see you with their medical questions. There was no infirmary on the ship, you were just sitting on a crate on the deck as various crew members told you more information than you cared to know. In fact, you’d prefer if none of them came to see you and left you the fuck alone. Despite that, you’d already seen seven of the crew members and dismissed them all when a seafoam green-haired man with eyeliner and lipstick walked up to you, already rubbing the back of his neck.
“Stop right there,” you said, holding up your palm to him. “Are you going to ask me about something that’s wrong with you?”
“Well, yeah-”
“Then here’s what I have to say before I hear the specifics. You need better quality jewelry for your nipple and dick piercings,” you said, holding out high quality stainless steel rings and bars in your hand. The man approached and took them gingerly from your palm, like you were going to bite him.
“Look - what’s your name?” you asked, squinting at the man.
“Boogie,” he replied, already taking off his shirt to change out the nipple piercing. You generated an iron ruler and rapped his forearm with the broad side.
“No! Bad Boogie!” you reprimanded as he squeaked. You reabsorbed the fan into your hand as you continued lecturing him, “That’s one of the reasons why everyone’s got skin infections! Wash your hands before you change jewelry!” He hung his head like a dog as you continued the same speech you’d given the five previous crew members to approach you.
“If you want to talk to me about your health, here’s the deal: I don’t need to see your penis. I don’t want to see your penis. We’ll get lotion for your rash, I don’t want to see that either. Everyone’s had pink eye recently, this ship is nasty. You’re assigned to cleaning duty along with everyone else. There’s nothing wrong with you so leave me alone. Does that cover everything you wanted to tell me?” you asked the sheepish-looking man.
“Yes, Ma’am,” he said with his head bowed.
“Don’t call me ma’am either, I’m not that old,” you scoffed, moving to sit cross-legged on the trunk. If only you ate the wine logia fruit instead, life would be so much better.
“Yes, Ma- Miss.”
“Go clean the ship, start with the bathrooms. This place is fucking gross,” dismissing your newest patient with a wave of your hand. You’d checked out the common bathrooms earlier that morning and found colors of mold you had never seen before. Maybe you’d turn yourself into an iron statue so you didn’t have to deal with these assholes anymore.You were still tired from being almost killed by hypothermia the night before and didn’t have a lot of patience left in you - what you really wanted was a nap.
“AND WASH YOUR HANDS!” you yelled at Boogie as he retreated below decks, his shoulders jerking at your shrill tone. “Goddamn imbecels, I can’t believe they made it this far without dying of fucking cellulitis,” you muttered to yourself. Looking over the side of the ship, you saw cannons sticking out on both sides of the ship, which piqued your interest.
Hopping off the crate, you stalked off to below deck before any other errant patients could find you to try to show you their genital piercings. You poked your head into various rooms on the port and aft sides as you walked down to where they kept their cannons - and more importantly, their cannonballs. Based on the amount of iron, you knew exactly where they were, but it was more fun to snoop through the ship.
Most of the rooms weren’t very interesting, containing food or supplies. You moseyed along, taking your time, until you felt a pull towards a room aft of the ship. It wasn’t the familiar draw of metal that you’d felt so many times before, but a latent feeling of magnetism that drew you closer. Kid wasn’t activating it, the pull was latent, so you walked towards the room to investigate. Maybe you could hide out and take a short nap just to regain some energy after the morning’s impromptu clinic.
The heavy door creaked open as you absentmindedly upgraded the metal on the hinges to prevent further noise. Inside was a workshop filled with projects at various stages of completion. You were guessing it was Kid’s but were willing to pay him a compliment even if it was. The number of projects in the workshop was staggering, you couldn’t calculate how many hours some of them would have taken - even for someone like you it was impressive.
Entering the room further, you inspected the metal hawk on the closest workbench. The metal was intricately wrought, on par with something you could create, possibly better. Each part of the bird was articulated, making the model even more lifelike. Even though one of the wings wasn’t complete yet, the hawk was still a breathtaking piece of craftsmanship. Leaning over, you began to notice the even finer details as you touched the bird gently with your fingertips.
Deciding not to be a dick for once, you left the workshop a few minutes later, closing the door behind you. Ok, so maybe Kid had one talent. And a gorgeous ass and an equally biteable body to go with it. That didn’t make you like him any better, he could still suck iron nuts. You continued to mull over the luscious body and horrible personality of Kid while you kicked in the next door. Ah, the artillery room, one of your most favorite on any ship.
Wandering over to the weaponry, you couldn’t help the scoff that escaped your lips. You rummaged through their cannonballs and didn’t find a single interesting item, only regular shot. You mentally deducted your compliment from Kid; having a boring artillery was one of the most grievous sins you could think of.
“Why the fuck don’t you have anything fun? This looks like a kid’s toybox,” you asked without turning around. Kid grunted from behind you as he leaned against the door jam. “No spider shot, no canisters, not even any shrapnel. Really, Useless, I expected better of you,” you sniffed.
“You got basic observation then?” he ground out as you insulted his lame ass artillery.
“I do, but you’re also loud as fuck stomping around in your dumbass boots. Don’t need to use it when my dickhead detection meter works just as well,” you snarked.
“Marines on the horizon,” he stated while cracking his knuckles in his palm. “Get ready to fight.” You scoffed as you picked up a particularly large cannonball for inspection.
“I’m always ready to fight, I’m probably the best you got on this ship right now. Maybe aside from Killer,” you said, running your fingers over the seam of the cannonball. You absorbed the metal and reformed it, making the single large shell now two hollow half spheres with a chain in the middle. The chain fit inside the ball so that it could be placed in the cannon and shot off. “See? Now that’s what I like to see,” you said with a broad smile. Kid scowled as you put the ball in the chamber of the cannon.
“You don’t even have a fire pit for hot shot? What a shame,” you tsked at Kid, shaking your head in mock disgust.
“Yeah, I see a hot shot right here,” Kid said, flashing the same grin you’d seen before he dunked you underwater.
“Don’t you fucking dare,” you hissed, already feeling the magnetic pull towards his metal arm. Kid intensified it, and your boots scraped against the wood floor as you became magnetized to his hand.
“Well, you told me my artillery sucks so I’m taking your advice, Squirt. You love to run that fucking mouth of yours, now I’m listening to your ideas like the good Captain I am,” Kid said, his eyes growing maniacal as he walked over to the window and opened it.
“Don’t. Fucking. Do. It,” you snapped as Kid reared back his arm. You wanted to punch him in the face so fucking bad but instead braced for impact - if your guess was correct.
“Let’s see whatcha got, Squirt. Back that attitude up with some action,” Kid said with a nasty laugh.
“I’M GONNA FUCKING KILL YOUUUUUUUU!” you screamed as Kid launched you at the incoming Marine ships. He had used a incredible amount of magnetic repulsion to send you speeding off towards the Marines, similar to a bullet shooting out of a gun. You turned yourself into a human-sized cannonball as you hurtled towards the Marine ship.
Wire POV
Wire was a little annoyed that he wasn’t going to fight the incoming Marines - everyone on the Victoria Punk enjoyed fighting, and especially fighting the Marines. When you fought against the World Government you could go all out and completely wreck, maim, kill, do whatever you wanted. Kid was known for his ruthlessness and Wire was happy to be a Commander on his crew.
But this was a close second. Kid had blasted you off like a rocket at those Marine ships as they sailed closer and Wire wished he had a recording snail for the event. You were absolutely relentless, decimating their ship and taking down the Marines all by yourself. When Kid had launched you, you’d turned yourself into a giant cannonball for the flight but quickly turned yourself into some kind of mess of chains and shrapnel as you hit the wooden deck with an enormous boom, the ship listing heavily with your impact.
“Don’t shove me, pussyface,” Wire grunted as he pushed back Rock, who was now jostling for a position against the railing for better viewing. The whole crew was portside, watching as the Marine ships crashed and burned - literally. You’d already punched a huge hole in one ship, which was rapidly sinking, and had launched yourself to the second of the three. It wasn’t a bad strategy, especially when outnumbered, Wire thought. The crew of the first ship was focusing on getting into small lifeboats or abandoning their ship, which was breaking in half. On the second ship, Marines were yelling and alternatively gathering for group melee while also being repulsed by your varied attacks.
“Holy fuck she’s mad,” Heat mumbled as they watched you turn your arm into a spiked mace to bash a Marine in the face and throw him into his friends behind him.
“I mean, ‘s fair. Kid fucking gunned her over there. Maybe Compo’s gonna be right and she’s gonna wreck our ship and drown us too,” Wire wondered aloud, pulling on a sideburn. He wouldn’t mind partnering with you during a fight, he thought, as you now projected iron spikes from your body into the attacking Marines. Turning your arms into giant maces, Wire winced as you crushed skulls and femurs without hesitation. He’d do the same but the mace seemed like an especially unpleasant method based on the screams coming from the ships
The Captain grunted as he polished some metal, seated on a barrel by the mast. He was pretending not to pay attention beyond a glance but Wire had known Kid for a long time. Kid was listening to the screams, and if Wire had to guess, enjoying it alongside the rest of the crew. He even picked his head up when a particularly loud scream ripped through the air to watch you thrust a serrated knife into someone’s throat.
Even so, the Marines vastly outnumbered you and were able to corral you towards the front of the ship. A few moments later and two Captains had you cornered against the bow, one some kind of lame devil fruit user and the other able to use armament haki. They were coordinating attacks, something that the Marines were often quite skilled at due to their training. Wire had been on the receiving end before and it could get ugly, fast.
The Devil Fruit user had some kind of paramecia umbrella fruit, able to produce umbrellas, which the other coated in haki to use as weapons. It was an interesting strategy, Wire thought, he’d never seen someone fight with sharpened umbrellas before. You were doing well, deflecting and attacking, but one of the Captains was able to stab at you with a haki-coated umbrella while other Marines attacked from behind. Some of the crew sucked in breaths or hissed as you bled out of a deep cut on your torso.
Kid’s eyes flicked from the gear he was polishing to you on the ship as you gripped your side, breathing heavily. You’d been doing well fighting about a hundred Marines on your own, but maybe it was time for some help from the crew. Kid’s arm was raised in a familiar battle stance, but he didn’t make any moves to assist you yet. Wire grabbed his trident from where it was leaning in preparation to board the vessels and get you out of there.
“Cap, that looks deep. Maybe we should -” Wire started to say before you turned yourself into a giant hammer and smashed both of the Marine Captains before they could react or coat themselves in armament haki. Wire frowned as brains and bone clung to your clothes, but your face was impassive as you turned back into your normal form. You sure fit in with the crew, even if you didn’t agree.
You were panting and leaned on the side of the ship in an effort to regain your breath, the remaining Marines scattering and fleeing on lifeboats. By that time, the remaining Marine ship had turned and was trying to get away. You shot them a dirty look but didn’t go after them, letting the ship retreat as fast as the wind would take them.
“BRING ME BACK FUCKWAD! THE SHIP IS SINKING!” you screamed, using a metal funnel to amplify your voice. Kid rolled his eyes but attracted you back to the ship, ass first. Wire had a fleeting thought that you’d turn yourself back into a cannonball for their own ship but you just plowed through several crew members on your way back to Kid, who had released his magnetic field as soon as you were on the ship. Compo wasn’t winning today but given your destructive tendencies, it still wasn’t a bad bet.
“Hope you enjoyed the show,” you said, your voice dripping with venom as you picked yourself out of the pile of crewmates who had been watching from the deck. You were clutching your side as blood dribbled through your fingers as you left to go below deck. Wire was thinking of asking if you wanted help but there were still scraps of brains on your clothes. Maybe later, he decided.
Your POV
You ambled off to the medical supply closet with as much dignity as you could muster, trying to stop yourself from limping. This wasn’t your first melee, certainly, but you were usually able to prepare yourself better for the ensuing battle. It was one thing to take into consideration the number of opponents, their positions, how they were configured, what Marine unit and level of specialization they were, and it was something completely different to be launched like a fucking beach ball at a Marine ship. Luckily they’d been C-class Marine craft – you didn’t know why they’d engage a Supernova like Kid anyway – but fighting 150 people on your own was tiring.
After eventually finding their medical kit, you opened the latches and prayed Killer kept it stocked. Throwing open the lid, you praised every god you could think of that there were suturing tools. You were tired and even though you could make your own forceps, it saved energy to use the ones they already had. Besides, you were going to have to sew yourself, which was draining enough. Not like you could trust any of the fuckos on board to do a good job if you were the one with the most medical experience.
You hesitated after taking the kit out of the supply closet, unsure where to go. The deck wasn’t somewhere you wanted to be right now - you were tired and didn’t want to talk to the gaggle of idiots topside. You’d go to the women’s quarters but you weren’t sure exactly where they were since you’d spent the previous night in Kid’s cabin. The sun was going to set soon and you wanted to find the closest room with natural light, finding it the best conditions for cleaning and closing wounds. Feeling the blood dripping down your shirt, you went to the room next door, which ended up being Kid’s workshop.
Shutting the door behind you, you set the kit down on an open workbench and began the process of preparing your workspace. You made a sterile metal tray and put the forceps, gauze, and rubbing alcohol on it before reabsorbing your shirt. The umbrella had been surprisingly sharp as it stabbed through your side, you’d been caught off guard. Luckily the speared tip had missed almost everything important but being skewered still hurt like a bitch.
You were standing in Kid’s workshop in your bra and wiping away blood from your wound with the rubbing alcohol when the door slammed open. You barely spared Kid a glance, as you could already feel the magnetic waves emanating from the world’s biggest tulip. There wasn’t much left in your tank and you needed to use it to clean and tend to your wound, not argue with an annoying dickhead.
“What’s up? You need me to get the last ship, too? Can’t take care of it yourself?” you said, now wiping the sides of the laceration to clean them of debris. Years of getting injuries prevented you from wincing but that didn’t mean it didn’t sting.
“You’re bleeding in my workshop,” Kid ground out, his eyes roving over your wound.
“No shit. Any other obvious things you wanted to tell me?” It wasn’t your best barb, but you weren’t focusing on Kid at the moment. “Fuck off and let me deal with it,” you said, setting down the now dark red cloth. You inhaled as you tried to remember if there were more gauze pads in the kit but drew a blank. Picking up the reverse cutting needle using the forceps, you leaned against the workbench and tried to find the best angle to watch your own work. It was annoying because your boob was kind of getting in the way of your vision and the laceration was a little towards your back - stitching it on someone else would have been easy but on yourself it was a little more challenging.
“Give me that,” Kid huffed, reaching for the needle. You yanked your hands away with a scowl.
“Not now. Can you just not be a total fucking freak for a few minutes? This is actually important,” you stated, grabbing the edge of the table for support. You were still bleeding and needed this done sooner rather than later.
“C’mere. I’m doing it,” he said, magnetising the needle to his hand. You balked immediately.
“No fuckin’ way, you’ll fuck it up and I’ll get gangrene and you’ll finally succeed in killing me. Just let me-” Kid tsked and crossed his arms. If your eyes momentarily flicked to his massive pecs who could blame you? You were wounded after all.
“Done this a million times. Me ‘n Killer do it for everyone. Stay put, don’t pussy out on me,” he said, already reaching for you. You were ready to argue again, but a sudden spell of dizziness had you closing your eyes and waiting for a moment. The sound of metal clattering to the floor had you opening your eyes as Kid swept his project over to the side but kept your tray where it was. “Lie here, it’ll be easier to work on ya. On yer side,” Kid said as he picked you up under the armpits like a child.
“H-hey, don’t do that,” you protested as your wound began to throb.
“Shut the fuck up and lay down,” he said, taking off his stupid red feathered coat and laying it on the table for you to lay on. You grimaced but did as he said, your blood dripping down onto the fabric. Kid grunted but didn’t say anything as he set down the forceps on the metal tray.
“You’re gonna need those-”
“Faster and more precise with magnetism. Hold still,” Kid said, focusing now only on the wound in front of his eyes. You took a deep breath as the needle pierced your skin, actively working on keeping yourself from turning into metal. Kid’s hand hovered over you as he intently watched the needle work its way in and out of your skin. It was a little weird to have his face so close to your side that you could feel his breath, but you didn’t want to break his concentration by mentioning it.
To his credit, Kid was efficient, the needle working much more rapidly than you’d be able to do it by hand. You closed your eyes and very soon he was tying off the last stitch, the wound sutured shut. Hopping off the workbench, you wavered a little before righting yourself. Kid’s metal arm was behind you as you were able to stand up straight.
“You gotta sanitize that, yanno,” you said with a frown as Kid replaced the materials within the first aid kit.
“Next time,” he replied, slamming the case shut. You kicked your foot against the foot of the workbench, feeling a little out of sorts. It was his fault you’d gotten the injury in the first place, so you didn’t really need to thank him. Still, it was a little better than having to sew yourself up.
“Coulda done it myself,” you said with a roll of your eyes. Kid grunted as he moved his goggles from his forehead down to his eyes and began pulling his projects back into place in his workbench. He was sorting through the objects and sorting them into piles, obviously preparing to use them in some kind of way. You stood there a few moments in silence, watching as gears and pieces began floating around his body, like a metal aura. It was a little mesmerizing, your fingers itched to touch the magnetic field.
“What?” Kid barked as he began fitting pieces together. Flicking your eyes over the metal pieces, you reabsorbed a few gears he was about to use. Kid sighed heavily as he grumbled, “stop being a bitch for a fuckin’ min–” You wordlessly handed him back the gears, this time in high quality steel. Kid didn’t say anything but began tinkering with the new gears, fixing them into a long narrow frame.
“Is that for the bird?” you asked, sitting on a stool near the table.
“Yeah, for the underwings,” he replied, now focusing on welding two tiny pieces together. You sat in silence, now crossing your arms on his workbench and resting your chin on top of them. Even though you were bone tired, it was interesting watching Kid work. He was in his element, focusing entirely on the work in front of him. Neither of you said anything as you crafted him a few better quality versions of the metal pieces he was using and he magnetized them from your hands. Kid was really more of an artist in this capacity, you thought, the wing coming to life before your eyes.
After about an hour, your eyes slid closed as Kid began attaching the wing to the rest of the model. You’d earned the right, you thought as you listened to him tinker with metal. Soon Kid would kick you out and you’d go find the women’s quarters, but until then it was pleasant to hear the hum of Kid’s magnetism while you rested. The last thing you felt while you drifted off to sleep was the weight of a heavy coat being placed on your shoulders.
Taglist: @mfreedomstuff
#opposites of attraction#kid x reader#kid x you#eustass x you#eustass x reader#that ship is fucking gross#that's canon#Oda doesn't need to tell me#are the idiots learning anything?#I too would like to bash things I don't like with giant hammers#here's looking at you Orion#hammers included#op x y/n#x reader
40 notes
·
View notes
Text
Magic Bullets: The Antibiotic Story
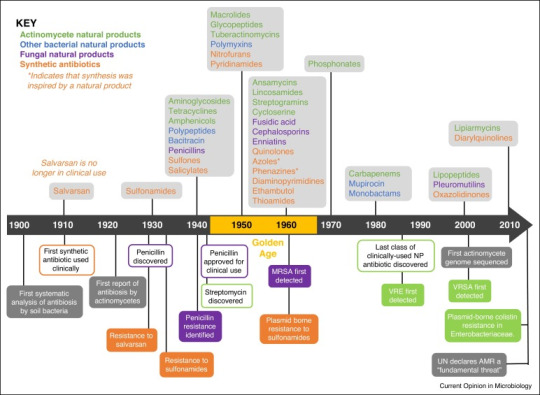
The year was 1907 and a Dr. Alfred Bertheim was trying to make arsenic less toxic to humans.
Why? Because in addition to killing humans, arsenic also kills trypanosomes- single-celled protozoa that cause the life-threatening infection trypanosomiasis. By creating a version of arsenic that still killed the protozoa, but not the human they infected, Dr. Bertheim could create a drug to treat the disease*.
This was not a fully new idea. About 50 years earlier, a drug called Atoxyl had been created in France. About 40 times less toxic than pure arsenic, it had been shown to not only successfully treat trypanosomiasis, but also the equally devastating syphilis infection.
But 40 times less toxic than pure arsenic is still not great. About 2% of people treated even one time with the drug ended up blind, among a myriad of other side effects. It was a start, but not ideal.
And Dr. Bertheim (under the direction of better-known Dr. Paul Ehrlich) was setting out to change that.
And it just so happened that the sixth compound from the sixth group he tried did so. Known as "compound 606", the new Arsphenamine could treat trypanosomiasis, relapsing fever, and syphilis very effectively- and it didn't leave its takers dead or blind.
Most of the time, at least. See, arsphenamine, also known by the brand name salvarsan, was a pain in the ass to administer. It had to be dissolved in several hundred mililiters of water under a nitrogen atmosphere to prepare it for administration. If it touched air, it would rapidly react, causing toxic byproducts that could cause liver failure, severe skin rashes, and even death.
But both trypanosomiasis and syphilis were definitely going to kill you, so it was worth the risk.
And the seed had been planted, so to say. The idea of a chemical able to kill infection-causing agents without killing the host was a true possibility for the future of medicine.
And by 1912, Neosalvarsan, a drug somewhat less effective -but far easier to administer and with significantly fewer side effects- was on the market. Over the next decade, Neosalvarsan would be responsible for a massive drop in syphilis cases worldwide.
But neither of the drugs could treat deadly infections from staph or strep or the hundreds of other bacterial or viral infections that still had no cure in the 1910's and 1920's.
Then came the first of the heavy-hitters. Bayer was a dye company when it started, and in 1932, three and a half decades after switching mostly to pharmaceuticals, chemists at Bayer were testing the company's dyes for anti-infective properties. They went through thousands of trials, finally finding a dye that could kill streptococcal bacteria without killing a mouse host.
Pre-1930s, streptococcal disease was a major problem. It caused strep throat, cellulitis, scarlet fever, childbed (purpural) fever, some forms of toxic shock syndrome, impetigo, necrotizing fasciitis, rheumatic fever, and many others. The skin infections may have been at least somewhat treatable with a hot compress, but the rest were prone to cause blindness, deafness, loss of limbs, and for many, loss of life.
In 1936, sulfonamide antibiotics changed that. Protosil, the first of the sulfonamides, became available to treat many of the infections listed above. These would be used for wound infections throughout WWII. Unfortunately, they would also cause the untimely death of nearly 100 people via the Elixer Sulfanilamide tragedy.
Sulfanilamide was a similar drug to Prontosil and was safe and effective for treating strep infections. However, when mixed with diethylene glycol (now used as standard car antifreeze) to make it into a liquid suspension, it was deadly. See this letter from a doctor who had prescribed the liquid form of the medication, not knowing it was poison:
[to read more about the Elixer Sulfanilamide Disaster, see here]
Despite the sulfanilamide tragedy, the race was on for more antibiotics. Three years before they went on the market, researchers had found evidence of bacterial resistance to sulfonamides. What would happen when these new bacteria, that didn't die when exposed to the new wonder drug, made up so much of the bacterial population?
In 1942, the Cocoanut Grove fire in Boston caused over 492 deaths and 130 injuries. The injured were among the first to receive a remarkable new drug called penicillin. The fire and the fate of the victims were publicized throughout the world, and penicillin became a household name overnight. But once again, even before it went on the market in 1943, just in time for the end of the Second World War, there was evidence of resistance.
But fortunately, the fire had been sparked. Over the next 30 years, many dozens of antibiotics would come into clinical use. If you've taken it, it probably came out between 1940 and 1970. Tetracycline, isoniazid, metronidazole, ciprofloxacin, erythromycin, vancomycin, amoxicillin, and dozens more you've never heard of.
And then? Nothing.
Well, not completely nothing, there were a couple that came out in the 1980s and a few in the early 2000s. But nothing like that 30-year golden age.
But now we're running into problems due to drug resistance. About 1.27 million people die annually directly from antibiotic resistant infection, while antibiotic resistance contributes to about 4.95 million more deaths.
The good news is that the drugs that are being made today are directly targeting those antibiotic resistant infections. In fact, as I'm writing this, a new drug (Zosurabalpin) is being tested for a bacteria called Carbapenem-resistant Acinetobacter baumannii, which up until now has had no antibiotic that works against it.
*as you may imagine for the time period, this was not necessarily a benevolent act. See, most of the reason Europeans wanted to treat trypanosomiasis in the first place was because they kept dying of it when they went to colonize Africa. And they wanted something that would give them a leg up on the people who were already there.
160 notes
·
View notes
Text

Comfort drawing of Onetrick
I have a skin infection (cellulitis) in my top surgery scars, I'm on antibiotics and have been getting better but I decided to finish this sketch to help me feel better ❤️
#digital art#art#oc artwork#character art#original character#oc#artwork#furry#mlp fanart#mlp#mlp oc#mlp art#mlp oc pony#mlp original character#my little pony#my litte pony friendship is magic#mlp g4#pony oc#pony character#unicorn#sona art
28 notes
·
View notes
Text

This is a heads up for my disabled, ADHD, fat, and chronically ill followers that may have to deal with injuries and topical infections! This stuff is awesome for if you have to look after a wound that you can't easily reach or clean multiple times a day.
Gentian Violet is a non-prescription topical antibacterial liquid that contains a blue skin-dying agent. My wound care doctor is fat, and his patients are largely bed-bound, bariatric, or otherwise can't keep up with rigorous wound-cleaning and bandaging routines for stuff like injuries or flareups of cellulitis infections.
This stuff stings pretty bad at first when it's applied and stains your skin a really potent blue color. Once the Gentian dries and dyes your skin, it means that you have a painted-on antibiotic membrane over your wound that you don't have to bandage, and keeps its seal on your wound for TWO DAYS. That includes with regular showering/bathing.
If you have memory issues, this stuff is fantastic. Not only does it stay active and killing bacteria for 2 days, but the reason the stuff is dyed so potently is so you remember to reapply it when the dye fades. When the dye starts to show your regular skin through again? Time too reapply!
If you have motion, mobility, or fatigue problems, this stuff is fantastic. Especially if you're looking after a wound that's in a tricky place to keep clean all the time without having to fully shower, you can literally use cotton swabs (no double-dipping, please! It's not sanitary!!!) to paint the area, and don't have to concern yourself with it again for another couple of days, giving you extra time to rest and heal, and more time to avoid feeling overwhelmed and panicked because you're "not taking good enough care" of it.
If you're allergic to bandage adhesives or get contact dermatitis from wound dressings, this stuff is great. Sometimes an injury or wound needs dressing just for the sake of the healing process rather than avoiding infection, but for ones where that isn't a concern for you, Gentian is a really good alternative for if Stuff That Cuts Off Air To Your Skin gives you problems.
All in all? It stings like hell at first, but my actual doctor told me that he regularly treats patients with full-limb wounds, and they suffer no ill effects for having large portions of their bodies painted with it instead of bandages and gauze.
If it seems like it might be helpful for you, please do talk to your doctor about it. In my state, it's non-prescription and my doctor gave me my bottle for free. Just be careful with using new medical products, and always remember that it's okay to say, "I can't do that easily. I'm disabled. Can you please provide alternatives for me?" when it comes to medical staff pushing you into care regimens that are more destructive than healing for you.
20 notes
·
View notes
Text
day off
Dude was in town for thanksgiving. it was supposed to be all of us but one of my nephews came down with walking pneumonia, which is apparently what all the kids are getting, so we didn't get the family thanksgiving. but dude came out, and programmed the thermostat in my cabin. i still think i'm going to mostly keep it shut off though. i'm getting low on propane and it's worrying me that it'll run out in the middle of the night sometime. it is 20F today though. and I have finally, with help, got my loom all ready and have started to weave the project i got all the stuff for last Christmas.
so i'm hanging out out here even though i could go inside and not be having to heat this space. so i'm like, not heating the space, even though it's slightly uncomfortable. it's up to 50F at the moment so i can't complain too much, the sun is out.
anyway-- I spent some time out here yesterday too and I got a bunch of work done both on the weaving and on the writing. I'm close to having enough of a first draft of the first bit of the tall ships solarpunk bisexuals novel that any of y'all who've expressed interest in reading will have something i can share with you soon. i just need to figure out where i'm heading.
i was going to put up more of the aubreyad fanfic too at some point but it's been so busy and then i just don't have any executive function. it's been rough.
oh also i got cellulitis again. i noticed a weird zit on my leg and in daylight i was like oh. that's an infection. what the fuck. never any broken skin but it managed anyhow. so i just immediately went to urgent care on friday morning when everyone else was meeting up to shop or whatever, and they were like oh well done for coming in this early, and gave me doxycycline. so i'm avoiding dairy for 8 hours a day now but you'd be surprised how much cheese you can eat around that restriction. i'm managing.
i also have to avoid sun but that takes zero actual effort this time of year. only a week of this left. the actual infection site looks fine but i'm of course giving it no quarter. i'm annoyed because i got several little cuts in my hands during all the hell of turkey processing and i was so good and so careful and none of THEM got infected so WTF. ugh.
I guess this season I'm thankful for doxycycline.
now, back to the solarpunk tall ship bisexuals, which keeps taking plot turns i had not anticipated and is not going where i expected. i think i'm also rambling too much but. y'know! we'll see.
the current scene that's rambling on far too long features the main non-sailor character realizing that she's inadvertently taught her nine-month-old to (in sign language) call the computer "daddy" because her father has been away at sea long enough that the child only remembers looking at pictures of him on the computer, and so now she requests screentime by making the sign for father. It is more or less her first word.
18 notes
·
View notes
Text
16 Wound Care Tips
DISCLAIMER: I’m not a doctor. The most medical advice you’re gonna get in here is ‘you should probably see a doctor if you see xyz’. I can’t definitively say if something’s infected or not, nor tell you about your specific circumstances.
TW for references to self-harm, and for somewhat graphic descriptions of wounds.
1. Your skin has 3 layers. The surface-level one is the epidermis; the white stuff beneath that is the dermis; and the yellowish stuff beneath that is the hypodermis. Any wounds that go deeper than the dermis need urgent medical care. Anything that goes deeper than the hypodermis is an emergency.
2. Deeper wounds are more likely to get infected than shallow ones. Unfortunately, deeper infections are also generally more dangerous than shallow ones. General things to look out for that signal infection are: redness; rash; a sense of heat in the wound; inflammation; red lines radiating from the wound; swelling; blistering; crust around the wound; impaired healing; pain; pus; and other discharge. (Note: a healthily healing wound may also produce some translucent-ish discharge. However, if the discharge is very yellow or very opaque, it’s time to see a doctor.)
2.5. One type of infection of the dermis or hypodermis is called cellulitis, and is a Very Bad Thing. As in medical emergency bad. As in will-spread-very-quickly-and-potentially-become-extremely-dangerous bad. Cellulitis usually looks like a red area (with soft borders), and tends to be painful to touch. Cellulitis can turn up anywhere on your body, but is most common on the legs.
2.75. If you have a fever with ANY of the aforementioned symptoms, go straight to hospital. Fever, in this context, tends to signal infection.
3. It’s better to kill an infection before it starts than to wait for symptoms. Wound care is best when it’s preventative. Wash your wounds - yes, even if they’re small - with water + soap, then use a topical antiseptic, such as povidine-iodine or chlorhexidine (that’s bepanthen). You can either get a dropper and drop it directly onto the wound, or get some gauze and swab it on yourself. Generally, covering this with a bandaid is a good idea, as it’ll stop stuff getting into the wound. If it’s relatively shallow, maybe you can get away with leaving it uncovered, but I’d err on the side of caution.
3.5. Do not put rubbing alcohol directly on your wounds - it’ll irritate the skin. However, if you are currently self-harming and seeking to minimise harm, rubbing alcohol can be used to clean any tools. (Clean before AND after, people!)
4. Some antiseptics and antibiotics are provided as creams or ointments. The difference between these is basically how much water they have in ‘em. Creams have more water, so rub into the skin. Ointments have less water, and sit on the wound instead of being rubbed into it. Don’t attempt to rub the ointment in and spread it thin as a result. You can be generous with ointment. Ointment is great, but will stain your clothes - so, it can help to cover it up with a dressing of some kind.
5. Wound dressings are anything you can put on the wound to stop stuff getting in. Wounds will heal faster if you cover them up - no, taking off the bandaid to ‘air it out’ will not, in fact, accelerate healing. Wound dressing options include (but are not limited to): bandages (good for when you need to apply pressure, which is to say anything deep); plasters (good for convenience); gauze + medical tape (more breathable, though I’m not sure of the benefits here). Change wound dressings at least once a day (unless otherwise instructed).
6. Bandaids and medical tape will leave adhesive on your skin. Wash it off with soap and water - otherwise, the sticky stuff builds up, and if you’ve got skin sensitivities, they might get flared up. If wound dressings are causing you continual flare-ups even when you wash the adhesive off, consider using a wound-prep wipe before dressing the wound (but consult with your doctor if it’s infected - I do not know the protocol here). And, for that matter, consult with your doctor anyway if you’re reacting to wound dressings - you might wanna get that checked out.
7. Your dermis contains some blood vessels, nerve endings, and hair follicles. If you hit a blood vessel, it will bleed a lot. So, if you see considerable bleeding:
If it is bright red and it spurts in time with your pulse, this is probably an artery. GO TO HOSPITAL IF YOU SEE THIS KIND OF BLEEDING. IT IS AN EMERGENCY.
If the bleeding is darker but more constant, you’ve probably hit a vein. If this doesn’t stop bleeding in 10 minutes, go to hospital. Put pressure on it in the meantime.
For the record, veins and arteries are not, in fact, bright red and bright blue like they are in textbooks. You will not know that you’re about to hit one until you do. Nerves are similarly difficult to see, but if an injury hits a nerve, it’ll be painful - either it’ll have an electric quality, a burning sensation, or it’ll sting like buggery.
8. The hypodermis contains: more nerves and blood vessels, as well as subcutaneous fat. Fat looks yellow and, uh, bean-like. If you see fat, it’s time to go to urgent care.
8.5. If you go below the hypodermis, go to A&E. I don’t care if it’s small - NOW.
9. Deep wounds may gape - that’s to say that they look, well, open. These wounds will heal quicker if you try to hold them closed to bring the skin walls together - that’s to say that steri-strips and butterfly bandages are your friend. Bear in mind that gaping wounds tend to be deep, so consider getting the wound looked at by a professional before trying to hold it closed at home.
Generally, after 48 hours, it’s unlikely that you’ll be given stitches, even if the wound was deep enough that it ought to have been stitched (that is: hypodermis or deeper). So, if it looks like it’s gonna need stitches (gaping or deep), go get stitches sooner rather than later. A good doctor or nurse will not judge you for whatever reason you’re seeking help.
10. Some skin areas are more prone to infection than others. (See: moist areas; legs; groin/lower abdomen.)
11. Don’t clean your wounds with tissue, paper towel, or toilet paper, as the materials tend to break up, and can leave a fun residue in the wound. Gauze swatches, cotton buds, and clean towels are your friend here.
12. Don’t put makeup on open wounds.
13. For deep wounds: in my experience with dermatillomania, these don’t tend to look like they fill in layer-by-layer so much as they just shrink/thin out. If it looks like it’s filling in in layers/healing slowly or healing in a way that’s incomplete, it’s time to see your doctor. For shallow wounds: if it darkens/goes yellow as it fills in, rather than scabbing, it’s time to see your doctor.
14. If you’re given a course of oral antibiotics, you need to finish the whole damn pack. Yes, even if you seem to have gotten better. Not finishing your dose, unless you’re specifically medically instructed to, may lead to the infection returning. Do not take that risk.
15. If antibiotics seem to be failing to clear things up, it’s time to see a doctor. Many funky things could be at play, but it’s not something you wanna take a risk on.
16. Check when you last had a tetanus shot. If you’re not sure, or if it’s since expired, get another tetanus shot.
6 notes
·
View notes
Note
Hi!
You mentioned in a recent post that an infected wound can develop into cellulitis, if I understood you right.
I'm curious - what is cellulitis? I don't believe I've run into that before (although might just be a language thing, English is not my first language and i don't often have a reason to know medical vocab in English haha), so I'd be grateful if you could tell me more about what it is and how it's treated!
thanks <3
Cellulitis is an infection of the dermal and/or subcutaneous layers (see the image below) of the skin that develops when a break in the skin introduces bacteria, most commonly group A streptococcus.
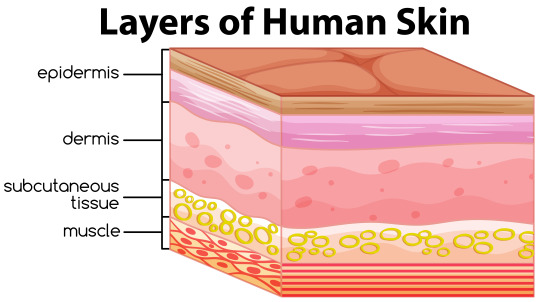
Cellulitis manifests as irregular reddened and swollen areas of the skin. Patients can also present with malaise, fatigue, and fever. Cellulitis is treated with oral antibiotics like cephalexin or clindamycin. If the patient has a fever greater than 100.4° F, a heart rate greater than 100 bpm, a breathing rate greater than 20 bpm, or an elevated white blood cell count, they will receive IV antibiotics.
Happy whumping!
2 notes
·
View notes
Note
ooo if you do combos - 20 & 45 with some Buck h/c?
thank you for the prompts! I hope you enjoy :)
When Eddie walks into the loft and sees Buck in nothing but a towel at the top of the stairs, he nearly drops his groceries.
But not in a fun way.
“Buck!” he scolds, hurrying to deposit the bags on the kitchen island. “What are you doing up? Why did you have a shower? You’re supposed to keep the stitches clean and dry!”
He catches Buck’s full-body eyeroll as he starts furiously putting things away in the fridge. This is exactly why Eddie dropped Chris off for an impromptu weekend with Pepa – he can’t leave Buck alone for twenty minutes before the man is already ignoring doctor’s orders.
“It’s been forty-eight hours,” Buck calls. “I’m allowed to get them wet now.”
“Forty-two hours!” Eddie shoots back.
Even from down in the kitchen, he can hear Buck’s scoff. “I don’t think six hours is going to make a huge difference, babe.”
Eddie scowls into the fridge as he places Buck’s oat milk on the shelf; he’ll be the judge of that, thank you very much.
It all started two days ago, when Eddie had roped Buck into helping him replace some rotting wood on Pepa’s front porch. The job itself had gone mostly smoothly – thanks in large part to Buck’s previous experience working construction – until the very end. Buck hadn’t been watching where he was walking, texting Bobby about something, and he’d stumbled right into the pile of old, rotten wood that they needed to dispose of. It had almost been hilarious, the cacophony of Buck swearing as the wooden planks bounced hollowly against each other, right up until Eddie had caught sight of the blood.
Buck had added a nasty cut to the collection of scars on his left leg. Eddie had cleaned it and dressed it as best he could in Pepa’s bathroom before taking Buck to the hospital for stitches, but he couldn’t shake the worry from the back of his mind about something nasty lurking on the decaying wood. His fears were proven warranted the next morning when Buck had gone to change the bandages and found the skin around the wound red and swollen.
After that, it was a trip to the doctor’s to confirm what Eddie already suspected: Buck had developed a mild case of cellulitis, because of course he had. Couldn’t just be a simple cut.
The doctor gave him a prescription for antibiotics to kick the infection and a list of at-home care instructions to prevent it from getting worse. Buck hadn’t been worried; Eddie, on the other hand…
Well. There’s a reason he insisted on staying with Buck.
He finishes putting the groceries away just as Buck comes down the stairs in a pair of sweatshorts and a t-shirt – his slight limp not going unnoticed by Eddie. Buck ambles over to the couch while Eddie washes his hands and then gathers the supplies the doctor sent them home with before scuttling over to join him.
When he drops to his knees between Buck’s legs, Buck’s eyebrows shoot up to his hairline. “Well hello,” he drawls.
“Don’t get excited,” Eddie says. “I need to cover your stitches.”
Buck huffs and slouches further into the couch, but obediently props his injured leg up on the coffee table. Eddie knows how irritated Buck can get being fussed over, and the fact that he lets Eddie mother hen him without complaint (mostly) makes Eddie’s insides go all fluttery. But that fluttery feeling flies out the window when Eddie runs his hand over Buck’s shin and finds the skin warm to the touch.
Shit, does Buck have a fever? If he does, that’s bad. That’s really, really bad. Eddie really tries to stop himself spiralling, but his mind can’t help but leap to worst-case scenarios: if Buck has a fever, that could mean sepsis, which could mean septic shock, which could mean organ failure.
Buck must read the panic on his face because suddenly there’s a hand on Eddie’s chin, gently turning him to meet Buck’s gaze.
“Do you feel any body aches or chills?” he blurts.
“Eddie.” Buck smiles softly at him. “I had a hot shower. That’s why I feel warm.”
“Right.” He lets out a long, slow breath, willing his galloping heart to calm down. “Right, yeah, that makes sense. Okay, I’ll bandage your stitches now.”
“Hmm, in a minute.”
Buck leans down, and Eddie pushes up on his knees to meet him in the middle. Their lips slot together gently as Buck’s hand slides around to tangle his fingers in the hair at the back of Eddie’s head, sending shivers cascading down Eddie’s spine. He lets himself get lost in the kiss, relaxing for the first time since he took Buck to the doctor’s.
Eventually, Buck pulls away, but not before planting a quick kiss on Eddie’s nose. “Thank you for taking care of me. But you seriously need to talk to Frank about your tendency to catastrophize.”
Eddie rolls his eyes, but doesn’t argue. Buck might have a point, given that it didn’t take much for Eddie to make the jump from warm skin to organ failure. He carefully covers Buck’s stitches with a new bandage before taping it in place to make sure nothing gets in to contaminate the wound.
“Thank you for letting me take care of you,” Eddie says, getting to his feet. “Now keep that leg elevated while I make us dinner.”
Buck shakes his head in fond disbelief, but reaches for the pillows without protest.
(also on ao3)
31 notes
·
View notes
Text

Chapter 4: Medical Esthetic Procedure Contraindications

So you’re considering getting some medical esthetic procedures done. That’s hot! But before you schedule an appointment or consultation here’s a quick guide of contraindications to be aware of!!

What is a Contraindication?
A contraindication is a condition we look for in the medical field that serves as a reason to not continue forward with a medical treatment due to potential harm the treatment may cause to a patient!
Laser Hair Removal:


Herpes and Cold Sores: Can you get laser hair removal with herpes or cold sores? Yes! But only if there is not an active breakout. We do warn the clients that the lasers we use are powerful enough to cause a herpes or cold sore breakout to occur so please proceed with caution!
Retinol: Use of Retinol’s are a huge no no! It can cause severe damage, burning or scaring if a laser is used! If you are on Retinol please stay off of it for 1 week before your laser hair removal procedure.
Seizures + Epilepsy: If you have a history of epilepsy please refrain from getting any laser or light treatment as it can induce seizures.
Bacterial Skin Infections: Infections can spread to other parts of the body if a laser is used.
Impetigo: This highly contagious superficial skin infection is something we as your medical esthetician should be aware of before continuing with treatment.
Cellulitis: This infection of the dermis and subcutaneous tissue should be cleared before you continue with any laser or light therapy.
Folliculitis: Laser treatments are not performed in areas of folliculitis but several hair removal lasers have been approved by the FDA for pseudofolliculitis barbae treatment.
Fungal Infections: Ringworm and Yeast Infections can not be treated with laser or light therapy until cleared.
Viral Infections: Active viruses are considered major contraindications for laser and light therapy.
Shingles: If there is an active outbreak laser treatment will not be used.
Common Skin Warts (HPV): Although some lasers are used to remove persistent warts, they are still considered contraindications.
Atopic Dermatitis (Eczema): You will not be disqualified as a candidate for laser treatment, unless the outbreak is in an area of proposed treatment.
Open Lesions, Rashes and Sunburns: This includes open lesions from picking at the skin. Any unknown lesions or rashes will be considered contraindications. Sunburns are known to disrupt the skin barrier and are considered contraindications. Any suspicious lesions should always be evaluated by a physician prior to treatment.
Accutane: You must be off of Accutane for at least six months to a year, depending on a physician’s  preference prior to treatment with laser or light therapy.
Immediate Post-Operative Face Lift, Blepharoplasty or Neck Lift: Treatment is avoided for clients who are in post op from these treatments until a physician has given approval for laser or light treatment. 
Pregnancy and Lactation: Pregnancy and lactation are considered contraindications women who are pregnant or lactating, should wait after pregnancy + breastfeeding so a child will not be exposed before beginning or continuing laser or light treatment. 
Laser Tattoo Removal:


Laser tattoo removal shares the same contraindications as laser hair removal.
Red Tattoo Ink: Red tattoo ink is known to be allergenic. If you have experienced an allergic reaction to red tattoo ink, be aware that another allergic reaction may occur if a red ink tattoo is being removed by laser. 
Retinol + Accutane
Pregnancy and Lactation
Bacterial Infections
Viral Infections
Fungal Infections
History of Epilepsy or Seizures
Open Skin Lesions, Sunburns and Rashes
Microneedling:


Herpes + Coldsores: Please wait until an outbreak is fully healed! Estheticians can avoid microneedling the mouth area if you do have an outbreak but it is best to wait until the outbreak is fully healed to avoid any spreading.
Active Acne: Areas of active acne can be skipped over but if there is an all over outbreak it is best to wait.
Rosacea: Clients with vascular rosacea can receive treatment, but not pustular or nodular rosacea wait until the information has settled.
Atopy, Asthma, Hay Fever and Allergies: Any patient with a history of allergies maybe prone to urticaria, after needling due to the release of histamines.
Anticoagulants: Any supplements, known to prolong, bleeding time, may not necessarily be discontinued from treatment, but the risk of bruising increases.
Drugs and Supplements Associated with Photosensitivity: Any drug and supplement that can cause photosensitivity including Accutane is considered a contraindication. 
Fitzpatrick III and Above: Those with darker skin tones are not disqualified from treatment but it should be known that skin will appear puffy, bruising, if present might be visible in thin skinned areas and erythema (skin redness)  when super-imposed on brown, appears much darker. Patience with melasma or post. Inflammatory hyperpigmentation must understand that lesions will appear darker for several months before improving.
PSA: There are certain ingredients to avoid using when it comes to dermal needling. Ingredients to avoid include preservatives, fragrances, emulsifiers, emollient acids, dyes, coloring agents, and UV filters 
Before receiving a dermal needling treatment, you may be asked by your provider about allergy or medication, history, blood pressure/medication, bleeding disorders, eczema, psoriasis, immune system disorders, keloid, scarring, major illnesses, heart conditions, anemia and a lot of other general medical questions.
Body Contouring


Pregnancy and Breast-Feeding
HIV/AIDS
All forms of Cancer
Undergoing Chemotherapy
Immunodeficiency
Lupus
High Blood Pressure
Uncontrolled Diabetes
Keloid Scarring
Excessive Pigmentation
Vein Inflammation
Steroid Medication
Chemical Peels + Laser Resurfacing
Sunburn
Recent Surgery or Scars: Wait 6 months
Open Lesions, Skin Diseases, Inflammation, Varicose Veins, Infection, Metal Implants, Metal Screws, Metal Contraceptive Coil + Prothesis/Silicone Implants: Area will be avoided
Antibiotics: Must wait until completed medication course
Depilatory Creams: Wait 2 weeks
IPL or Laser Treatment: Area that received laser or light therapy must wait 2 weeks before receiving body contouring.
Areas with Botox: Wait 3 months before receiving body contouring.
Areas with Dermal Filler: Wait 2 weeks before receiving body contouring.
Sun Tan: Will be avoided
Chronic Inflammation: Speak with your healthcare provider before proceeding forward with a body contouring treatment.
PSA: Before receiving body contouring, your hydration levels will be checked your body must be 40% or higher for your hydration level. Hydration levels below 40% can cause cat like scratch sensations when receiving body contouring. Which is why low levels of hydration are considered a contraindication and you must wait until your hydration levels are at 40% before receiving treatment.

30 notes
·
View notes
